Liposuction vs Weight Loss Surgery: What’s the Difference?
When people talk about changing their body shape or losing excess fat, the terms liposuction and weight loss surgery (bariatric surgery) sometimes get used interchangeably — but they are fundamentally different tools with different purposes, candidates, outcomes, and commitments. This article breaks down what each procedure is, who it’s for, how they work, when they can complement each other, and how to decide which (if either) is right for you.
1. What is Liposuction?
Liposuction is a cosmetic surgical procedure that physically removes localised fat deposits to improve body contour. It is not intended as a weight-loss solution for obesity; instead, it’s used when someone is already near their ideal weight but has stubborn pockets of fat that don’t respond to diet and exercise.
How it works
A surgeon makes small incisions and uses a cannula (thin tube) to suction out fat from targeted areas such as the abdomen, thighs, hips, arms, or neck. There are variations (e.g., power-assisted, ultrasound-assisted, laser-assisted) designed to optimize fat removal and skin retraction.
Ideal candidates
Good candidates for liposuction are:
-
Adults within roughly 30% of their ideal body weight with firm, elastic skin and good muscle tone.
-
People with localised fat deposits (not generalised obesity).
-
Healthy individuals without serious medical conditions that impair healing, and ideally non-smokers.
Benefits
-
Immediate improvement in body shape.
-
Relatively quick recovery compared to major surgery (depending on extent).
-
Can be combined with other cosmetic procedures.
Limitations and risks
-
Not a treatment for obesity; it does not produce significant systemic weight loss or metabolic improvement. Fat can return in other areas if lifestyle isn’t maintained.
-
Common complications include contour irregularities, bruising, swelling, and in large-volume cases, higher risk profiles — although overall liposuction is considered safe when performed by experienced surgeons. Safety standards and guidelines (training, patient selection, documentation) are maintained by specialist bodies to reduce risk.
Recovery
Compression garments are typically worn for weeks to optimise contour and reduce swelling. Most people return to light activities within a few days and fuller activity over several weeks depending on extent.
2. What is Weight Loss (Bariatric) Surgery?
Weight loss surgery, also called bariatric or metabolic surgery, is a medical intervention aimed at treating obesity and its related health conditions by altering the digestive system’s anatomy and physiology. It leads to substantial and sustained weight loss and often improves or resolves comorbidities such as type 2 diabetes, hypertension, sleep apnea, and fatty liver disease.
Common types
-
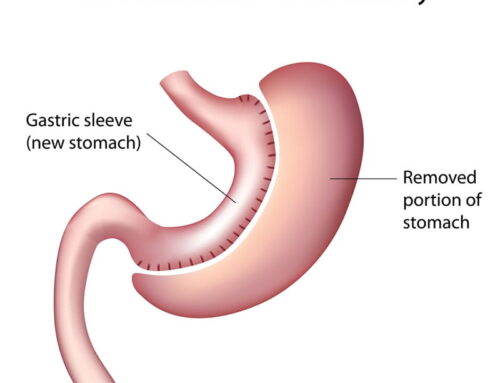
Gastric sleeve (sleeve gastrectomy) – removes a portion of the stomach to reduce volume and affect hunger hormones.
-
Gastric bypass (e.g., Roux-en-Y) – creates a small stomach pouch and reroutes the small intestine, reducing absorption and appetite.
-
Adjustable gastric band – older technique involving a band around the stomach (used less now).
-
Other metabolic procedures (e.g., mini-gastric bypass) are also evolving based on guidelines.
Mechanism
These surgeries do more than restrict intake: they cause metabolic and hormonal changes that reduce hunger, alter satiety signalling, and improve insulin sensitivity — contributing to durable weight loss beyond simple calorie restriction.
Candidate eligibility
Contemporary international guidelines (e.g. ASMBS guidelines) recommend bariatric surgery for:
-
Individuals with BMI ≥ 35, or
-
BMI ≥ 30 with at least one significant obesity-related comorbidity (e.g., type 2 diabetes, hypertension, sleep apnea).
Some programs (and evolving guidelines in parts of the world) allow consideration with BMI 30–35 if metabolic disease is present, and thresholds may be adjusted for ethnicities that develop comorbidities at lower BMI.
Australian context emphasises a multidisciplinary assessment and long-term follow-up, with primary care and specialist teams collaborating to optimise outcomes.
Benefits
-
Significant, sustained weight loss (often 25–35% of total body weight maintained long-term).
-
Improvement or remission of obesity-related diseases (e.g., diabetes, high blood pressure).
-
Reduction in all-cause mortality in appropriate candidates.
Risks and commitment
-
It is major surgery and carries risks (nutritional deficiencies, surgical complications, need for lifelong supplementation, possible weight regain if follow-up/lifestyle falters).
-
Requires a commitment to dietary changes, supplementation, psychological support, and regular medical follow-up.
Surgeon and centre experience matters
Outcomes, including complication rates and durability of benefit, are significantly better in high-volume surgeons and centres with standardised postoperative pathways. The surgeon/centre volume-outcome relationship is well-documented for bariatric procedures, with lower complication rates and more consistent long-term results associated with experienced teams.
3. Side-by-Side Comparison
| Feature | Liposuction | Weight Loss (Bariatric) Surgery |
|---|---|---|
| Primary goal | Body contouring / cosmetic fat removal | Treat obesity and metabolic disease with sustained weight loss |
| Mechanism | Physical suction of localised fat | Anatomical and hormonal alteration of digestive system |
| Typical candidate | Near ideal weight; good skin tone; localised stubborn fat | BMI ≥40 or BMI 35–39.9 with comorbidity (some expanded criteria apply); clinically severe obesity |
| Weight loss magnitude | Usually modest; not intended for systemic weight reduction | Substantial and durable (often 25–35% of body weight) |
| Systemic health impact | Minimal (cosmetic only) | Improves or resolves comorbidities (e.g., diabetes, hypertension) |
| Recovery | Days to weeks | Weeks; plus lifelong lifestyle follow-up |
| Risk profile | Low in properly selected patients; contour irregularities possible | Higher upfront risk but lowered in experienced centres; includes nutritional and surgical risks |
| Long-term maintenance | Patient-dependent; fat can return in untreated areas | Supported by metabolic changes but requires adherence to follow-up and lifestyle |
| Surgeon volume effect | Important for aesthetic outcome and complication avoidance | Strong evidence that higher-volume surgeons/centres have better outcomes |
| Common combination | Often done after massive weight loss for fine-tuning | Can precede liposuction if needed for excess skin / contour |
4. When They’re Used Together
Many patients undergo bariatric surgery first to achieve major weight reduction and then, once weight stabilises and excess skin or residual localised fat remains, consider liposuction or body contouring (including abdominoplasty, arm lifts, etc.) to refine shape.
This staged approach respects the limitations of liposuction for weight loss while leveraging its strength in aesthetic refinement after the metabolic and weight benefits of bariatric surgery have been realised.
5. Questions to Ask Your Surgeon
Before committing to either procedure, ask:
-
Experience and volume: How many of this specific procedure do you perform per year? Do you work in a high-volume centre (especially relevant for bariatric surgery)?
-
Complication rates: What are your personal and institutional complication rates? How do you handle complications if they arise?
-
Candidate suitability: Why do you think this procedure is appropriate for me? Are there alternatives?
-
Expected outcomes: What realistic results can I expect, and over what timeline?
-
Recovery and commitment: What is the recovery plan? What lifestyle changes are required before and after?
-
Long-term follow-up: For bariatric surgery, what does your multidisciplinary follow-up involve (dietitian, psychologist, medical monitoring)?
-
Combination planning: If I need body contouring after weight loss, how is that staged?
6. Frequently Asked Questions
Q: Is liposuction the same as weight loss surgery?
A: No. Liposuction removes localised fat for contouring and does not address obesity’s metabolic or systemic aspects; weight loss surgery alters the digestive system to produce substantial, sustained weight loss and improve health conditions.
Q: Can I have liposuction if I’m obese?
A: Liposuction is typically not recommended as a primary treatment for obesity. Candidates should be near their ideal weight with localised fat deposits. For significant obesity, bariatric surgery is the evidence-backed path.
Q: Will bariatric surgery get rid of all my fat?
A: Bariatric surgery leads to major weight loss, but residual skin or localised fat may remain; some patients later choose liposuction or body-contouring procedures.
Q: Does the surgeon’s experience matter?
A: Yes. For bariatric surgery there is strong evidence that high-volume surgeons and centres have lower complication rates and better long-term outcomes. The same applies in aesthetic surgery (including liposuction) where experience improves contour results and reduces issues.
Q: Can I have both procedures?
A: Yes — most commonly bariatric surgery first for weight loss and metabolic benefit, followed later by liposuction or other contouring once weight is stable.
7. Summary & Next Steps
-
Liposuction is best for refining shape when you’re already at or near your goal weight.
-
Bariatric surgery is a powerful medical intervention for treating obesity and improving related health conditions.
-
Many patients benefit from a combined, staged approach: metabolic weight loss first, aesthetic refinement later.
-
Choosing the right procedure starts with the right candidate assessment and an experienced surgical team.
If you’re unsure which path fits your goals and health profile, book a consultation at Mastakov Surgery. Together we can review your weight history, body goals, medical background, and develop a tailored plan — whether that’s metabolic surgery, contouring, or both.