Weight-Loss Medications in Australia: What’s Available Now, How They Work, and the Pros & Cons
Weight-loss medication has changed fast in Australia. These medicines can help reduce hunger, improve fullness, and support
steady weight loss when used with a structured lifestyle plan. This guide explains what’s available now, who it may suit,
how each option works, side-effects to know about, and practical next steps.
Quick summary
- Most modern options act on gut hormones that control appetite.
- They work best with diet, activity, sleep, and ongoing clinical support.
- Not everyone will respond the same. Safety checks and follow-up are vital.
- If medicines don’t suit—or weight returns—bariatric surgery offers the most durable results for many people with obesity.
How do weight-loss medicines work?
The leading options are incretin-based therapies. They copy or boost gut hormones that signal fullness and slow stomach emptying.
You feel satisfied sooner, eat less, and your blood sugar control improves. A newer class acts on two receptors at once for a stronger effect.
- GLP-1 receptor agonists – reduce appetite and slow gastric emptying.
- Dual GIP/GLP-1 agonists – target two pathways for additional appetite and metabolic control.
- Other agents – reduce fat absorption, curb cravings, or act as appetite suppressants.
What’s available in Australia right now?
Availability can change due to supply and regulatory updates. Your clinician will confirm what’s appropriate for you and whether
it’s prescribed for weight management or for another indication (like type 2 diabetes) with off-label weight-loss benefits.
| Medicine (Class) | How it works | Dosing | Typical Result* | Common Side-effects |
|---|---|---|---|---|
| Semaglutide (GLP-1) – brands include Ozempic (T2D) and Wegovy (weight management) | Signals fullness, slows gastric emptying, supports glucose control | Weekly injection with gradual dose increases | Many patients achieve 10–15%+ body-weight reduction over time* | Nausea, reflux, constipation/diarrhoea, fatigue; rare pancreatitis |
| Tirzepatide (dual GIP/GLP-1) – brands include Mounjaro (T2D) and, in some regions, an obesity-label | Activates two incretin receptors for stronger appetite and metabolic effects | Weekly injection with step-up dosing | Often 15–20%+ weight-loss in trials* | As above, plus possible injection-site reactions |
| Liraglutide (GLP-1) – Saxenda | Similar to semaglutide but shorter-acting | Daily injection with up-titration | ~5–10% body-weight reduction for responders* | Nausea, vomiting, diarrhoea, headache |
| Phentermine – brands include Duromine / Metermine (appetite suppressant) | Stimulates the central nervous system to reduce appetite | Daily capsule; usually short-term use | Can support several kilograms of loss in the first months* | Insomnia, dry mouth, palpitations; not for people with certain heart conditions |
| Naltrexone/Bupropion – Contrave | Acts on appetite and reward pathways to reduce cravings | Oral tablets; dose escalates over 4 weeks | Modest average loss; works best with lifestyle plan* | Nausea, headache, insomnia; avoid with certain meds/conditions |
| Orlistat – Xenical (Rx) / Alli (OTC 60mg) | Blocks absorption of ~25–30% of dietary fat | Take with meals containing fat | Modest extra loss when diet is maintained* | Oily stools, urgency, flatulence—reduced if dietary fat is kept low |
*Results vary widely. Figures above reflect ranges reported in clinical studies for responders when combined with lifestyle support.
Pros and cons at a glance
Incretins (GLP-1 & GIP/GLP-1)
Pros: Strongest average weight loss; weekly dosing; benefits for blood sugar and heart risk in some patients.
Cons: GI side-effects common at the start; supply/cost issues; injections; not ideal with certain conditions.
Best for: People needing larger, steadier loss with medical support.
Phentermine
Pros: Oral; lower upfront cost; useful short-term for appetite reset.
Cons: Stimulant-type effects; sleep and heart-rate issues; generally time-limited.
Best for: Short bursts of support in selected patients without cardiac risk.
Naltrexone/Bupropion
Pros: Oral; can reduce cravings and snacking.
Cons: Nausea, headache; interactions; slower response.
Best for: Emotional or reward-driven eating when stimulants aren’t suitable.
Orlistat
Pros: Long safety record; oral; OTC version available.
Cons: GI side-effects if dietary fat is high; modest effect size.
Best for: Patients wanting a non-stimulant, non-hormonal option with disciplined diet.
Who is a good candidate?
- Adults with BMI ≥ 35, or BMI ≥ 32 with weight-related health issues (e.g., T2D, sleep apnoea, hypertension).
- People ready to pair medication with nutrition, activity, sleep, and behaviour change.
- Those able to attend regular reviews and blood tests.
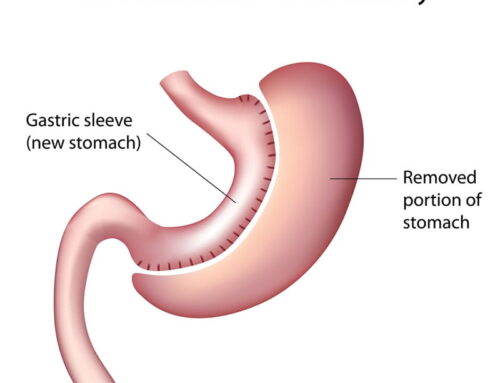
If your BMI and health risks are higher—or you’ve tried medication without lasting success—gastric sleeve
or gastric bypass may offer greater and more durable weight loss. We discuss your full set of options at consult.
Safety, side-effects, and precautions
All medicines can cause side-effects. We screen carefully and start at low doses with slow increases. Tell us about all medicines and supplements you take.
- GI symptoms like nausea, reflux, bloating, constipation, or diarrhoea are common early with incretins. These usually settle with gradual dosing, smaller meals, and hydration.
- Gallbladder issues can occur with rapid weight loss; report upper-right abdominal pain.
- Pancreatitis is rare but serious: sudden severe abdominal pain needs urgent care.
- Low blood sugar can occur if combined with certain diabetes medicines.
- Phentermine may raise heart rate or blood pressure and disturb sleep—unsuitable for some cardiac conditions.
- Naltrexone/bupropion interacts with several drugs and isn’t appropriate with seizure disorders or uncontrolled hypertension.
Costs, access, and supply
Costs vary by brand, dose, and whether your prescription is for diabetes or weight management. Some medicines may be subsidised for diabetes but not for obesity.
Supply can fluctuate. If a product is unavailable, we’ll discuss safe alternatives or bridging plans.
Medication vs surgery: which is right for me?
Medication
- Good for moderate weight loss and metabolic control.
- Flexible and reversible; can pause or switch.
- Effect often linked to ongoing use.
Bariatric surgery
- Most effective long-term option for significant obesity.
- Improves or resolves many weight-related conditions.
- Requires commitment and structured follow-up.
We’ll help you weigh up medical therapy, surgery, or a staged plan (medicine first, surgery later if needed).
How Mastakov Surgery supports you
- Comprehensive assessment – medical history, labs, medications, goals, and lifestyle.
- Clear education – simple dosing calendars, side-effect tips, and food guides.
- Dietitian and nursing follow-up – habit coaching, accountability, and long-term monitoring.
- All options on the table – if medication is not ideal, we discuss sleeve and bypass with transparent pros and cons.
What to expect at your first appointment
- Discuss your weight history, medical conditions, sleep, and medicines.
- Review goals (health, mobility, fertility, energy, confidence).
- Choose a plan: lifestyle alone, medication, surgery, or a combination.
- Set up follow-up: dose increases, food plan, symptom tracking, and blood tests.
Ready to explore medical weight-loss?
Book a consultation in Brisbane, Gold Coast, or Hervey Bay. We’ll tailor a safe plan you can stick to—and we’ll be with you for the long haul.
FAQs
How much weight can I lose with medication?
It depends on the medicine and your biology. Incretin-based medicines can produce double-digit percentage loss for many responders. Others provide modest loss that still improves health markers.
How long do I need to stay on it?
These medicines manage appetite signals. If you stop, appetite may return. Some patients stay on therapy long-term; others use it to build habits and then taper.
Are these medicines safe?
They are generally safe when prescribed after a proper assessment and monitored closely. We review your history, medicines, and blood tests, then start low and go slow.
Can I use medication before or after surgery?
Yes. Medication can help pre-op weight loss and is sometimes used post-op if weight begins to climb. We individualise this plan.
What if supply is limited?
We’ll discuss alternatives, dosing strategies, and timelines so you’re never left without guidance.