Gastric Bypass vs Gastric Sleeve (2025 Comparison)
Not sure whether a sleeve or bypass is right for you? This guide compares results, reflux/diabetes outcomes, risks, recovery, vitamins and costs—so you can discuss the best fit with your surgeon.
Book a consultation · Learn more about Gastric Sleeve and Gastric Bypass
Quick summary
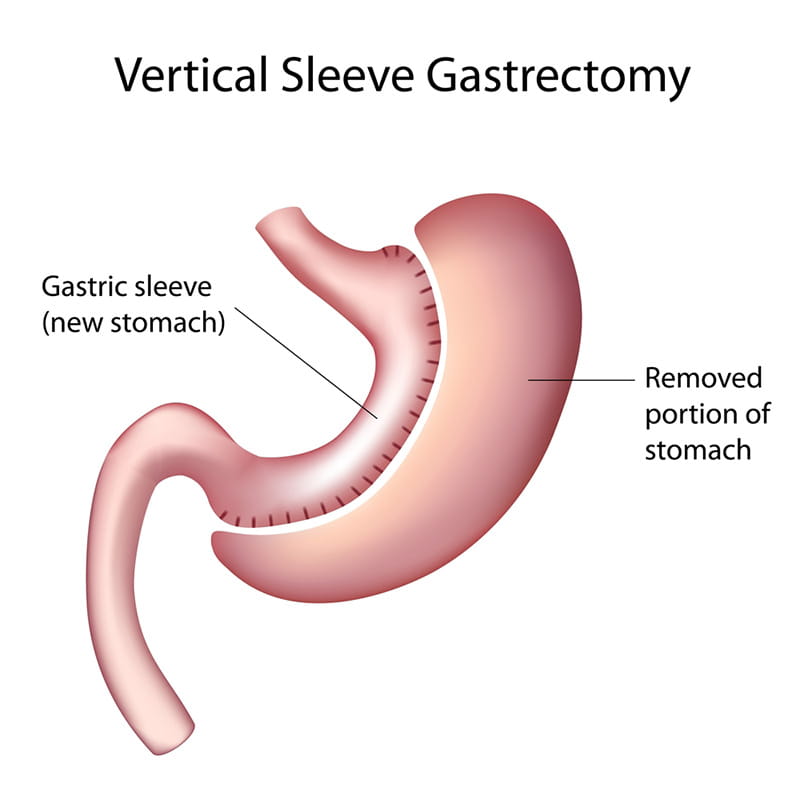
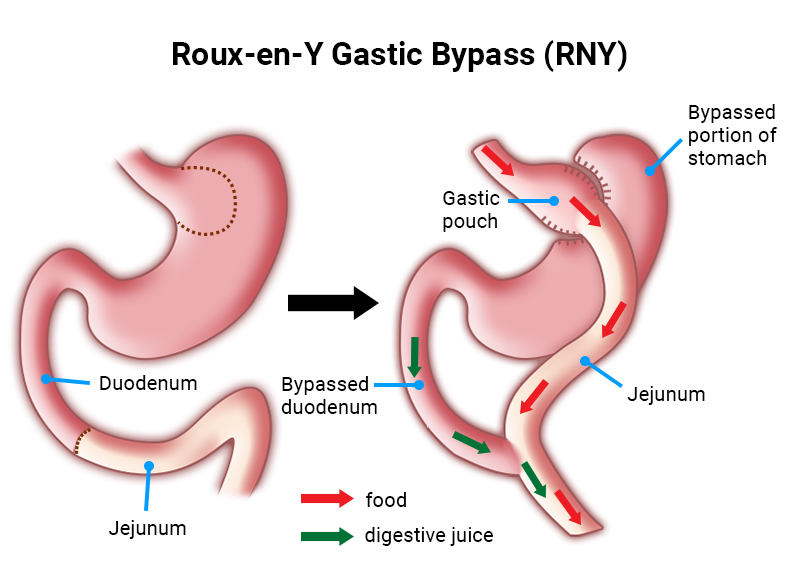
Gastric sleeve removes ~75–80% of the stomach to create a narrow “sleeve”. It limits portion size and reduces hunger signals. Gastric bypass (Roux-en-Y) creates a small stomach pouch and reroutes the small intestine; it reduces intake, modestly reduces absorption and changes gut hormones—often helpful for reflux and diabetes.
Side-by-side comparison
| Factor | Gastric Sleeve | Gastric Bypass (Roux-en-Y) |
|---|---|---|
| Typical weight loss* | ~25–30% total body weight at 1–2 years (with program support) | ~30–35% total body weight at 1–2 years (with program support) |
| Type 2 diabetes effect | Improves insulin sensitivity; some remissions | Higher chance of remission/improvement |
| Reflux/heartburn | Can worsen or newly appear in some | Often improves reflux symptoms |
| Dumping syndrome | Uncommon | More common (after high-sugar meals) |
| Ulcer risk with NSAIDs/smoking | Lower than bypass | Higher—avoid NSAIDs; smoking increases risk |
| Vitamins & minerals | Lifelong supplements recommended (B12, iron, ± Ca/D) | Lifelong supplements essential (B12, iron, Ca/D) |
| Endoscopy access | Normal upper-GI access | Altered anatomy; access to bypassed stomach is limited |
| Reversibility | Not reversible; can revise to bypass/SADI-S if needed | Considered permanent; some revision options exist |
| Hospital stay | Usually 1–2 nights | Usually 2–3 nights |
*Individual results vary. Long-term success depends on follow-up, nutrition, movement and support.
Which is better for…?
- Problem reflux or large hiatus hernia: Bypass often preferred.
- Severe diabetes/metabolic syndrome: Bypass may offer stronger metabolic effect.
- Lower surgical complexity & normal anatomy: Sleeve is simpler, keyhole procedure.
- Need for ongoing NSAIDs (e.g., arthritis): Sleeve may be safer—bypass has higher ulcer risk.
- Future endoscopy of the whole stomach required: Sleeve preserves normal access.
See detailed pages: Gastric Sleeve · Gastric Bypass.
Pros & cons
Gastric Sleeve — advantages
- Good weight loss with simpler anatomy than bypass
- No intestinal rerouting; normal upper-GI access
- Shorter operating time and hospital stay on average
Gastric Sleeve — considerations
- Reflux can persist or appear in some patients
- Lifelong vitamins and regular blood tests recommended
- Revision may be needed for inadequate weight loss or reflux
Gastric Bypass — advantages
- Often better for reflux and diabetes improvement/remission
- Strong, durable weight-loss outcomes
- “Dumping” can discourage high-sugar intake (for some this is a positive)
Gastric Bypass — considerations
- Higher risk of marginal ulcers with NSAIDs/smoking
- Dumping symptoms after high-sugar meals (manageable with diet)
- More demanding vitamin/mineral replacement long-term
Risks & safety
All surgery carries risk. Potential issues include bleeding, infection, leak at staple lines/joins, blood clots (DVT/PE), strictures and nutritional deficiencies. Bypass can also have internal hernia or marginal ulcers; sleeve can worsen reflux in some. Your personalised risk is discussed during consultation, and we use pre-op assessment, experienced technique and structured follow-up to reduce risk.
Learn more: Sleeve risks · Bypass risks
Recovery & diet
- Stay: sleeve 1–2 nights; bypass 2–3 nights
- Back to desk work: typically 1–2 weeks (varies)
- Diet progression: Fluids → Purees → Soft → Regular over ~4–6 weeks
- Supplements: long-term vitamins/minerals (B12, iron, ± calcium/vitamin D)
See details: Sleeve diet stages · Bypass diet stages
Costs & rebates
Out-of-pocket costs vary by health-fund cover, hospital/anaesthetic fees, and aftercare. You’ll receive a personalised quote after your consultation.
Learn more: Sleeve cost · Bypass cost · Costs & finance
How to decide
- List your goals (weight, reflux control, diabetes management).
- Review medications you must keep (e.g., NSAIDs) and any reflux/hernia history.
- Discuss pros/cons with your surgeon and dietitian.
- Choose the option that best fits your health profile and lifestyle.
Next steps
Book a consult to review your history and choose the safest, most effective option for you.
Book a consultation · Local pages: Gold Coast · Brisbane · Hervey Bay
Information is general and not a substitute for medical advice. Outcomes and recovery vary.
Sleeve vs Bypass — FAQs
Which is better for reflux?
Bypass often improves reflux, whereas sleeve can worsen reflux in some people.
Which is better for diabetes?
Both help; bypass tends to show higher rates of remission/improvement.
Can I take anti-inflammatories after surgery?
Regular NSAIDs raise ulcer risk after bypass. Sleeve may be safer if you need ongoing NSAIDs.
Is either procedure reversible?
Both are considered permanent. Revisions are possible in selected situations.
How do I choose?
Match the procedure to your goals and health profile (reflux, diabetes, medications), then confirm with your surgeon after a personalised assessment.
